Cortical Motor Mapping
Electrophysiological brain mapping is performed as a necessary adjunct in surgery to clarify the relationship of brain tumors to functional regions of the brain. Mapping is most commonly performed during surgery to identify areas in the brain responsible for body movements (primary motor cortex, precentral gyrus or the Rolandic area) as well as language (Broca’s or Werneckie’s areas) (Figure 1). Although all areas of the brain are functionally active, some may be considered dormant or redundant in function with other anatomical areas. In these regions, manipulation of the brain incurred during surgery or brain injury resulting from stroke, trauma or bleeding may result in only temporary disability or a deficit may be undetectable. Operative resection of these areas do not benefit from the use of brain mapping.
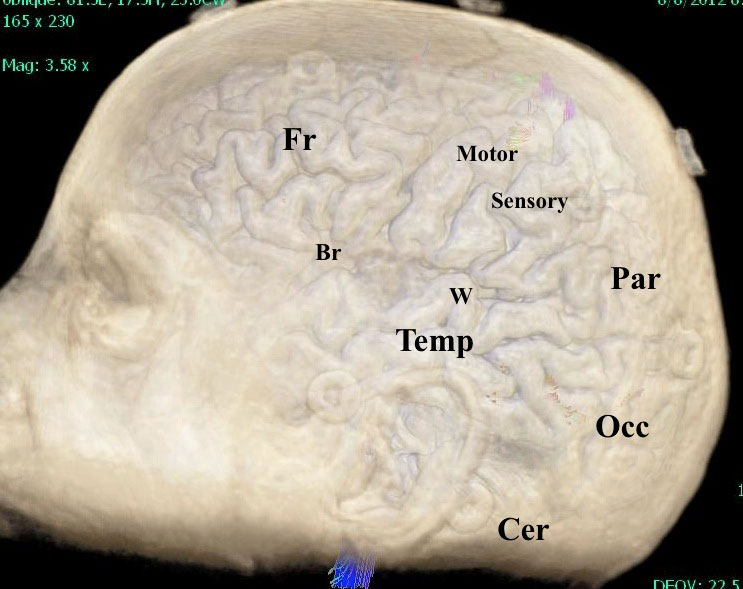
This three dimensional MR rendering demonstrates the relative location of the Frontal (Fr), Temporal (Temp), Parietal (Par), Occipital (Occ) lobes and Cerebellum (Cer). Broaca’s (Br) and Werneckie’s (W) language areas are indicated and the primary motor and sensory cortex are labeled accordingly.
Alternatively, certain areas of the brain sometimes referred to as ‘eloquent cortex’ forms a nexus of function which if injured will result in permanent and irreversible injury. These areas control language and motor function and require a consideration for mapping either together with or independent of pre-operative functional MR and diffusion tensor imaging. For mapping of the motor cortex, a patient may be either fully anaesthetized or conscious during surgery. In the fully anaesthetized patient, stimulation with a defined electrical current is applied directly to the brain’s surface and a response is measured from electrodes placed in the face, arm, and leg by a neurophysiologist and is easily observed as a muscular contraction. Alternatively, motor mapping may be accomplished in a conscious patient with the patient self-reporting in real time the present or absent effect of stimulation.
Cortical Language Mapping
Mapping areas of the brain responsible for language may only be performed with a conscious patient able to participate in exercises during surgery. Tasks may include reading, interpreting printed images, responding to verbal cues, counting or general conversation. Stimulation with an electrical current in these circumstances usually results in an arrest of speech. Resumption of function normally resumes after the stimulus is removed.
Importantly, ‘awake’ surgery does not imply that an anesthesiologist is not present or that medications are not administered. Rather, the patient is fully asleep during the exposure and closure of surgery. When the surgeon has completed the exposure and is prepared to begin mapping and tumor resection, the patient slowly regains consciousness to participate in language and recall exercises. Medications are continuously administered during the conscious part of the procedure to control pain, anxiety, nausea, and to render the patient generally amnestic for the intra-operative period.
Subcortical Stimulation and Localization of the Corticospinal Tract
The primary motor cortex (figure 1) is located at the most posterior part of the frontal lobe and is responsible for initiating movement on the opposite side of the body. The multitude of electrical impulses that allow us to will movement are delivered by ‘axons’ which are an elongated part of a brain cell or neuron that is specifically designed to conduct electricity. Axons from the primary motor cortex are bundled together and form the ‘corticospinal tract’ and travel through the deep part of the brain to the brainstem and spinal cord (figure 2). The tract dissipates as nerve fibers deliver information to secondary neurons that in turn form the nerves traveling through the face, arms and legs. The corticospinal tract cannot be distinguished from other parts of the brain by the naked eye or with the aid of an operating microscope and for this reason tools have been developed to prevent its injury. The use of diffusion tensor imaging sequences linked with intra-operative navigational equipment is limited by brain shift and other technical errors in accuracy. Intra-operative electrical stimulation beneath the surface of the brain, ‘subcortical stimulation’ allows for a prediction of the distance and direction of this fiber tract reliably.
Localization of the motor cortex on the surface of the brain may be performed by cortical stimulation or by other techniques. Once the outer surface of the tumor is identified by navigation systems, ultrasound or direct visualization the resection begins. As the surgery proceeds, stimulation of the perimeter of the tumor at its interface with the surrounding brain is performed and is increased until a response is elicited from the electrodes inserted into selected muscles of the face arm and leg. The magnitude of this stimulus is an indicator of the distance to the corticospinal tract. As the resection proceeds, a lesser stimulus will be required to obtain a comparable response and indicates the directionality and distance to the fiber system. This technology is a powerful tool in allowing for maximal resection of primary brain tumors that tend to be infiltrative and have an indistinct interface with the brain.
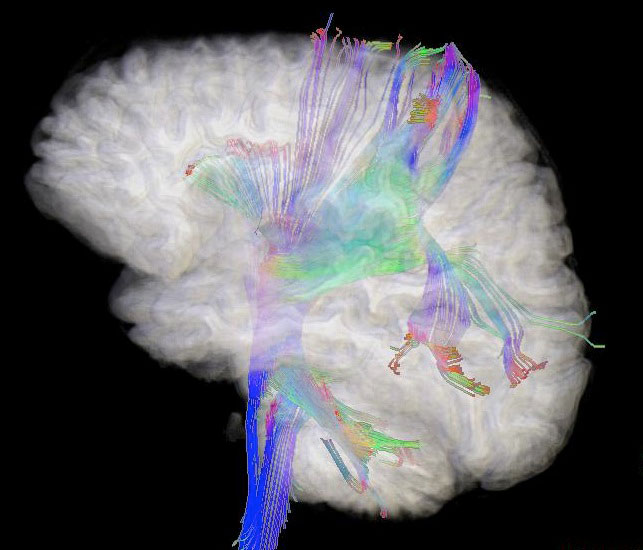
Figure 2 – MR diffusion tensor imaging demonstrating the axonal bundles within the brain.