When Should You Consider Spine Surgery for Your Back Pain?
 Are you among the 40% of Americans who have experienced back pain in the past year or among the 80% who have experienced it at some point in their lives? If so, and conservative treatments haven’t helped you, it’s natural to begin to wonder if spine (back) surgery is necessary.
Are you among the 40% of Americans who have experienced back pain in the past year or among the 80% who have experienced it at some point in their lives? If so, and conservative treatments haven’t helped you, it’s natural to begin to wonder if spine (back) surgery is necessary.
While there’s not a simple answer to this question, many back pain sufferers may be able to avoid surgery.
Given that I spent seven years and hundreds of hours in a surgical residency perfecting the technical skills required to perform minimal access and open spine surgery, it may seem ironic that I view surgery as a last resort. But that’s the philosophy I have come to embrace over the years.
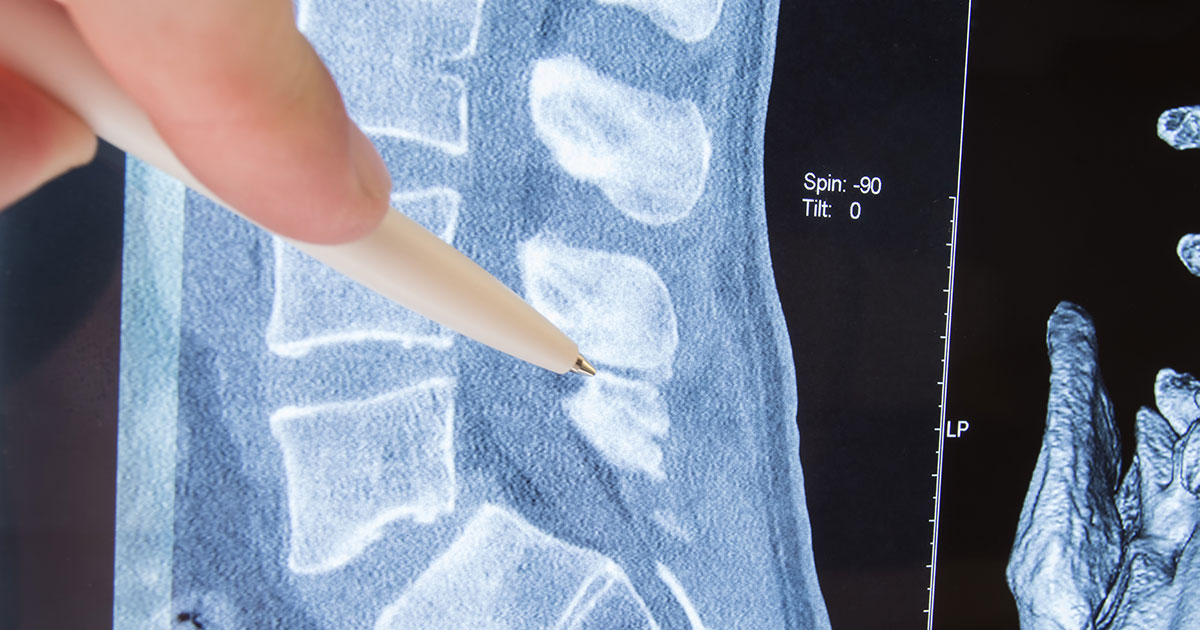
Shortly after I began practicing neurosurgery, I experienced severe back pain myself. An MRI showed that I had both a herniated L5-S1 disc and spondylolisthesis (where a vertebra slips forward onto the vertebra below it) caused by a stress fracture I likely had gotten years before when playing football. My neurosurgeon peers all recommended that I get surgery, but I didn’t want to be sidelined for the weeks it would take to recover.
As my career matured, I began to consider my own experience with pain and the experiences of my patients, and I began to recognize that our perception of pain is very much influenced by how we contextualize that pain. And, I began to realize that my prowess as a surgeon depends not just on understanding where pain originates, but also how each patient responds to pain.
I began to see that we should view ourselves as adaptable, rather than vulnerable. When we have that attitude and the right guidance, we can often learn to properly stress our bodies through exercise and experience the miracle of adaptation. This may reduce our pain and allow us to avoid surgery.
How do you know that you are with the “right” surgeon? When you meet with a spine surgeon, if you feel you’re not getting adequate communication about your treatment options, get another opinion.
I’ve heard patients say, “I don’t care about my surgeon’s personality. Just give me a good pair of hands.” I couldn’t disagree more. Most surgeons are technically capable but it is their character that counts. There is a big difference between being able to perform a procedure and taking the time, energy, and effort to do it well. It is your surgeon’s character, more than skill, that will assure that result.
In the years I’ve been practicing and continuing to learn, I’ve found that the best way to take care of people is to put myself in their shoes. I ask myself what the patient would choose if they were to have my fund of knowledge and experience, and make my recommendation from this perspective.
If a surgeon tells you that you “need” surgery, I suggest that you walk out of his or her office. Too many surgeons focus on being the hero or showing off their surgical skills. I recommend looking for a surgeon that can tell you the pros and cons of different approaches to treating your pain. He or she should educate you and then help you to make that decision. The term “need” is self-serving and rarely appropriate. Our culture has predisposed people to think that, if their back hurts, there’s something broken and they need intervention – often first through pills or injections and then through surgery. They want a quick fix for their pain so they can move on with their lives. But for most patients, the decision to have back surgery is gray, not black and white. Talk with your surgeon about the chances of your pain getting better if you wait. Ask what happens if you do nothing. Ask about PT. Likewise, ask what you can expect if you get an injection. And ask about surgery. If the nerve compression is due to a disc herniation, patients can get better without surgery in the overwhelming number of cases. That said, surgery is the right option for some patients. The factors that tend to move you to surgery include anatomical conditions such as osteoarthritis that results in bone spurs, which can create insufficient room for one or more nerves to pass through openings in your spine and that won’t improve over time. Other factors that may make surgery an appropriate option include:
Generally speaking, the more that the available space in the spinal canal is permanently compressing the nerves, the more likely it is that surgery will result in a positive outcome.
Strengthening the hidden core muscles of your back could be key to reducing your pain. While encouraging more movement may seem counterintuitive, the proper approach can work wonders.
Some exercise regimens today focus on strengthening the front of the core, the transversalis muscle in your abdominal area. But that’s only half the story, and studies have shown that doing this can cause an asymmetry that may even weaken the back. By contrast, the approach I recommend in my book focuses on strengthening the entire back – the front, the sides, and the back-like a brace, to create a natural weight-lifting belt. Key to this is strengthening the posterior chain of muscles in your back – especially the multifidus muscles deep in your lower back, which I call the ‘hidden core.’ Strengthening it can stabilize the spine, reducing motion which in turn reduces pain and helps you harness the synergy between your body and your brain.
Instead of viewing pain as an indication that something is ‘broken,’ I teach my patients how to relax when they start to feel pain and educate them that the pain is often a reaction to something that can be controlled. I call this replacing panic with equanimity.
I start each patient visit by determining if I can decipher what’s generating the pain. If not, I turn to a mind-body approach and teach my patients to see themselves as adaptable. Education is an important determinant of health – if you learn about your physiology and anatomy, that will help you have better health going forward.
Remember, your health is something you have to acquire rather than something you hope to be blessed with. How you eat, sleep, exercise and handle stress is very important. Patients instinctually avoid activity in order to avoid pain, but I encourage them to exercise so that they paradoxically will experience less pain. Walking (or running) is an essential part of health acquisition. If your back pain is preventing you from walking to get healthy, I’m likely to recommend a more aggressive treatment approach.
We live in a quick fix society. But there is no quick fix for most back pain. I encourage my patients to lean into a slow fix. Learn as much as you can, and learn how to be comfortable without black and white answers. Having a surgeon who has your best interests at heart is a great start.
For more information about my approach to back pain, visit my website where you can learn more about the two books I’ve written on the topic: The End of Back Pain and The Me in Medicine.