This non-radiation-based diagnostic study was developed in the 1970s and was widely distributed in the 1990’s and offers a precise view of brain and spinal anatomy. MR is an indispensable study to all neurosurgical disciplines including spinal surgery, neuro-oncology and neurovascular. Patients at times develop a level of anxiety during the study. This sense of confinement may be treated with medications to relieve anxiety; newer magnets furthermore offer more space for patient comfort without sacrificing image quality.
Functional MR imaging (fMRI)
This MR modality allows anatomical localization of centers of language and motor function and is useful as an adjunct to intra-operative brain mapping in preparation for surgery (Figure 1). To obtain useful imaging, patients are prepared and coached before the study to perform either simple tasks such as finger or foot tapping to localize motor function or verbal exercises to pinpoint centers of language. Tasks are then performed while the patient is positioned in the MR during the acquisition of the study; subtle differences in regional cerebral oxygen utilization are measured while the patient is at rest and while the task is performed. These studies may be lengthy and require a patient’s full concentration and focus. Results may compel the treating neurosurgeon to consider other forms of treatment such as Gamma Knife radiosurgery if tumors are located in manifestly functional area of the brain.
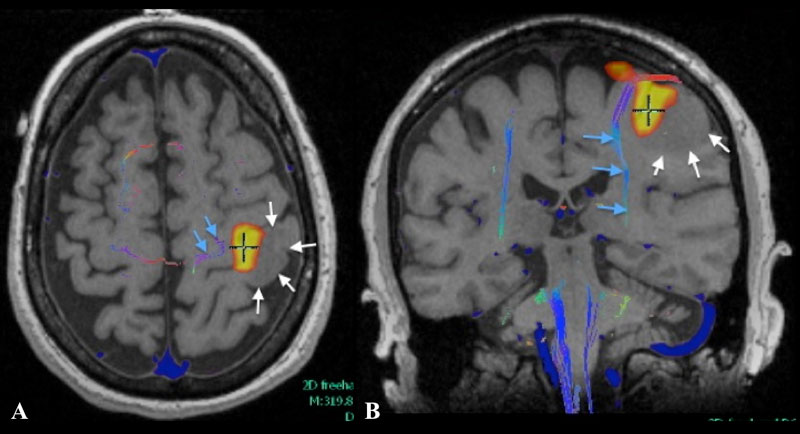
Figure 1: Axial (A) and coronal (B) T1 weighted MR fMRI localizing hand function with relation more laterally placed hypo-intense neoplastic process (white arrows) with more medially situated descending motor fibers of cortico-spinal tract as indicated by MR tractography
Diffusion Tensor Imaging (DTI)
This MR sequence is performed primarily to identify the location of the bundle of neuronal fibers that descend from the brain through the brainstem and spinal cord to subserve motor function. Of primary interest is an understanding of the relationship of a tumor with these fibers. Preservation of these fibers is tantamount to prevent paralysis or weakness
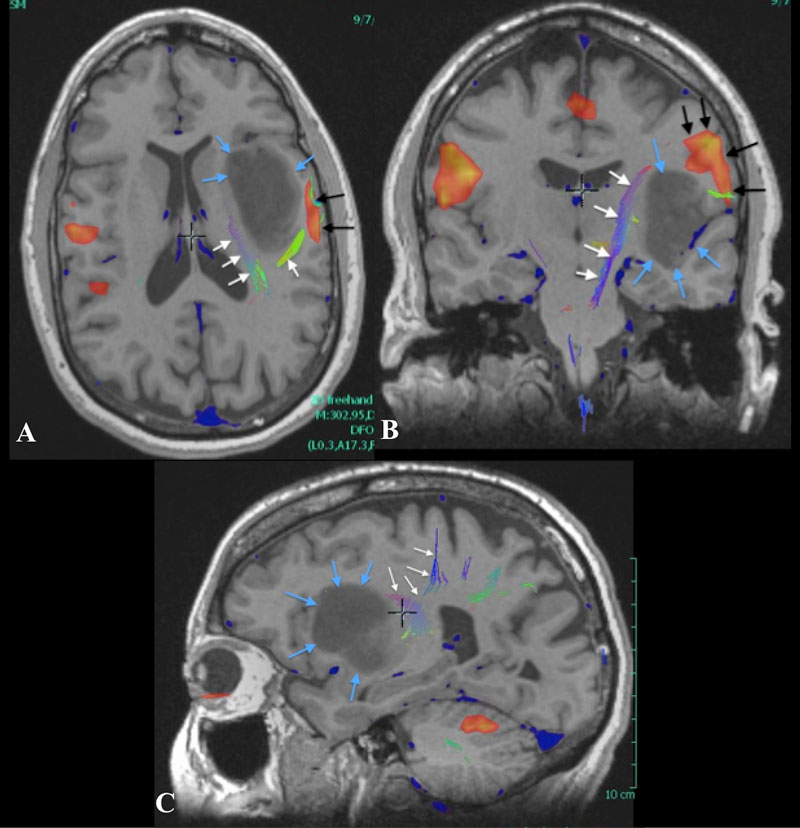
Figure 2: Axial (A), Coronal (B) and Sagittal (C) plane T1 weighted MR images with superimposed functional data demonstrating the lip and tongue area of the motor cortex (black arrows) as well as the more medially placed corticospinal tract fibers(white arrows). Tumor located in the insular cortex (blue arrows).
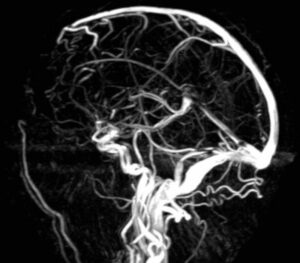
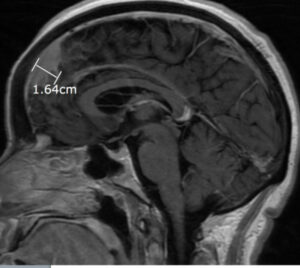
MR Angiography or Venography (MRA, MRV)
This MR modality allows for a non-invasive assessment of the arterial and venous structures of the central nervous system and provides an understanding of the interrelationship with tumor anatomy.
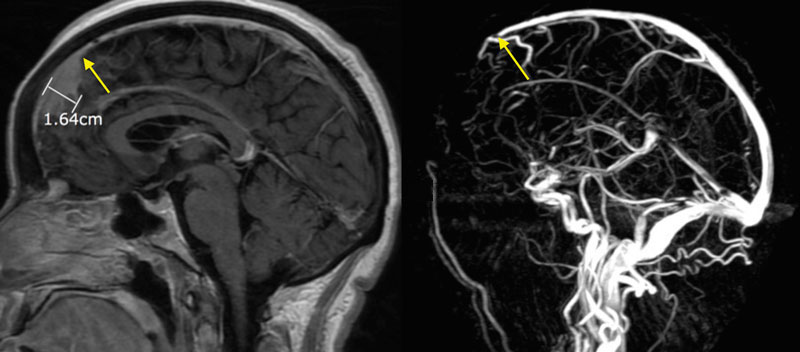
Figure 3
(Left) Sagittal post contrast T1 weighted MR showing a parasagittal meningioma invading the superior sagittal sinus (yellow arrow). (Right) MRV demonstrating absence of venous blood flow (yellow arrow).
MR Spectroscopy (MR SPECT) and perfusion imaging
These MR sequences are obtained in an effort to help define the nature of an abnormality seen on standard anatomical MR. Spectroscopy and perfusion imaging enable doctors to distinguish with some accuracy between tumor, infection or an area of necrosis (dead tissue). These studies represent the initial foray of medicine into the concept of a virtual non-surgical biopsy.