Skull-base tumors are by definition located underneath the brain in difficult-to-reach areas and are intimately associated with vital and delicate neurovascular structures. Surgical resection is often necessary to alleviate mass effect and brain swelling associated with larger tumors. Radiosurgery, however, is a viable and comparatively safe alternative that has been shown to arrest tumor growth and in a minority of cases to induce tumor contraction.
Meningioma and vestibular schwannoma are but some of the tumors that benefit from this modality with literature demonstrating lasting control over years of follow up. Although the procedural risk associated with radiosurgery is exceedingly low, tumor progression and delayed complications in the form of cranial nerve injury and radiation induced brain swelling are known to occur in a proportion of patients.
Case Study #1 – Gamma Knife Radiosurgery for Vestibular Schwannoma
Patient is a 75 year old woman presenting with symptoms of gait ataxia and progressive cognitive decline with initial imaging demonstrating communicating hydrocephalus with a 2.8 cm right sided vestibular schwannoma (figure 1a). There was no distortion of the ventricular system as a result of tumor mass effect (figure 2). Patient underwent high volume lumbar puncture with improvement in balance and CSF protein was elevated.. She underwent a left occipital VP shunt with resultant improvement in symptoms and Gamma Knife radiosurgery. Imaging obtained four months later demonstrate diminished central enhancement reflecting treatment effect (figure 1b) and 16 months later there has been a measurable decrease in tumor size (figure 1c). The patient continues to do well and functioning independently.
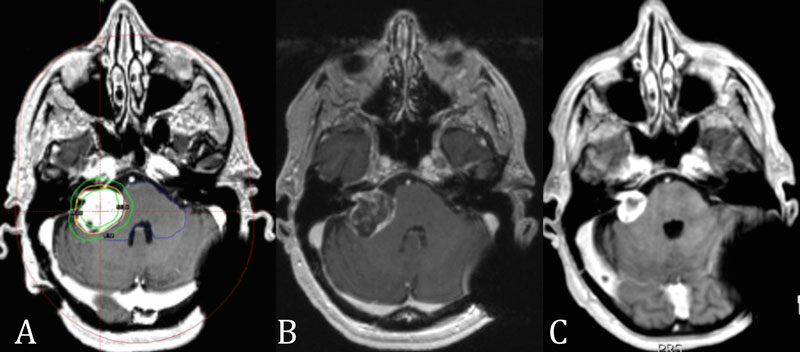
Case 1 – Figure 1
A: Planning axial T1 weighted post contrast MR image shows a large right sided vestibular schwannoma measuring 2.8 cm with distortion of the middle cerebellar peduncle. B: Image at 4 months post treatment showing decrease in tumoral enhancement. C: 16 months post treatment there has been a contraction of tumor volume and mass effect.
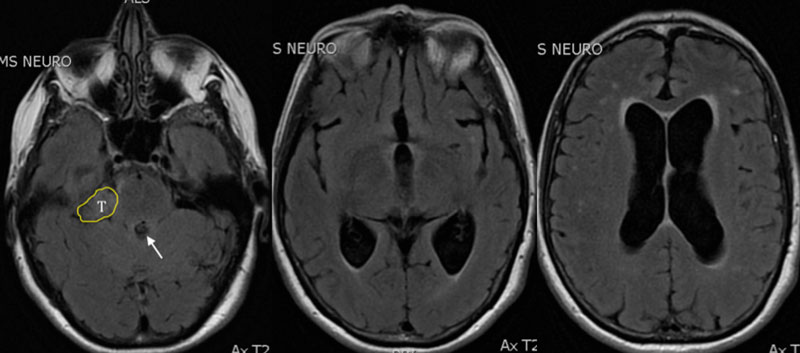
Case 1 – Figure 2
Pre treatment imaging shows hydrocephalus without obstruction of ventricular system (arrow) by tumor (T, yellow perimeter).
Case Study #2 – Gamma Knife Radiosurgery for Tentorial Meningioma
Patient is a 75 year old man with a two year history of V1 trigeminal neuralgia with MR imaging demonstrating a left mesio-tentorial meningioma with distortion of the brainstem at the trigeminal nerve root entry zone (Figure 1). Serial imaging demonstrated no evidence of tumor growth but pain was persistent and severe despite maximal medical therapy. He was treated with radiosurgery using a dose of 12.5 Gy to the 50% isodose line and noted improvement in pain within two months after the procedure (Figure 2).
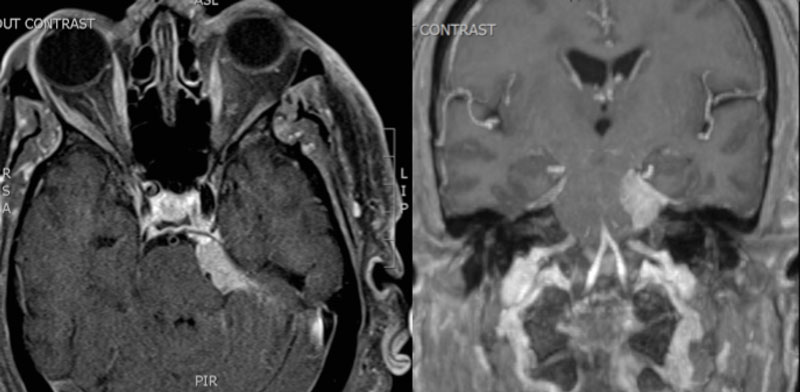
Case 2 – Figure 1
Axial (left) and coronal (right) demonstrate an enhancing extra-axial mass at the level of the petrous apex and Meckels cave with distortion of the brainstem at the trigeminal nerve root entry zone.
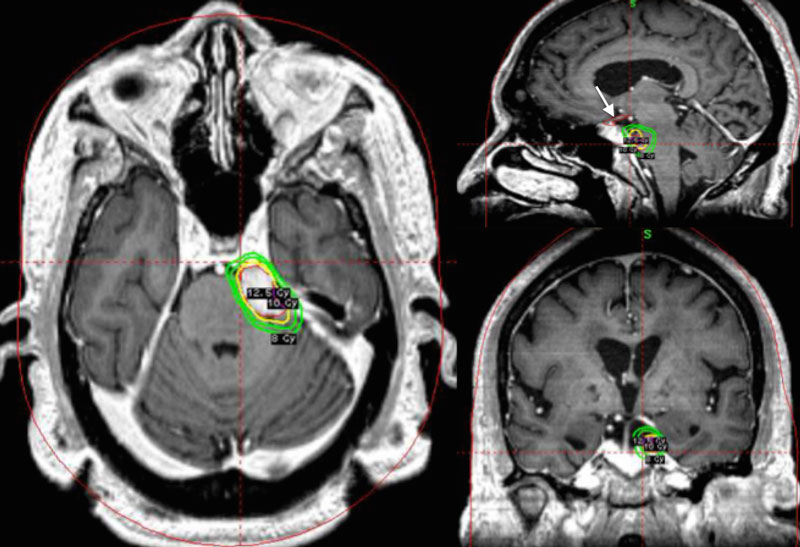
Case 2 – Figure 2
Treatment plan MR imaging showing contoured tumor border (yellow line) as well as 12.5, 10 and 8 Gy isodose lines (green lines). The optic nerves/chiasm were also contoured (red line indicated by white arrow) to assure that they were appropriately shielded from an unacceptable dose of radiation.