Our multidisciplinary team of surgeons are experts in treating cerebral vasospasm, strokes, brain aneurysms, and rare arteriovenous malformations (AVMs). As all of these conditions are life-threatening, it is important to seek immediate treatment at the onset of symptoms.
What is vasospasm?
Vasospasm occurs when blood vessels narrow, constricting blood flow and oxygen delivery (see Figures 1, 2). Often, local inflammation following a ruptured brain aneurysm narrows arteries, and, in major cases, can limit or completely disrupt blood flow to areas of the brain, causing another stroke.
While vasospasm can occur anywhere in the body, there are two primary types: cerebral vasospasm (within the brain) and coronary vasospasm (affecting the coronary arteris of the heart).
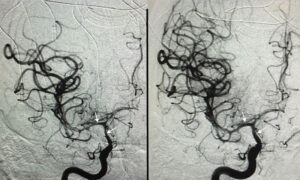
Figure 1
Left: AP angiogram showing vasospasm of the internal carotid, middle cerebral and anterior cerebral arteries (arrows). Right: AP angiogram after treatment with balloon angioplasty showing an increase in the diameter of vessels (arrows).
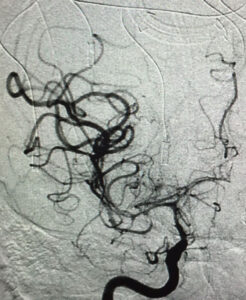
Figure 2
Superimposed images more clearly demonstrating the benefit of balloon angioplasty in treating vasospasm.
What causes vasospasms?
Cerebral vasospasm is most often caused by a subarachnoid hemorrhage following the rupture of a cerebral aneurysm. Vasospasm occurs in up to 20% of patients within 4 to 14 days of aneurysmal subarachnoid hemorrhage. Ideally, these patients are monitored closely for the first two weeks following surgery, as the delayed complications related to ischemic stroke – such as paralysis, loss of the ability to speak, or coma – may occur after an otherwise uneventful aneurysmal clipping or coiling.
Less frequently, vasospasm may be inadvertently caused by surgical manipulation or medicinal side effects.
What are the symptoms of vasospasm?
Vasospasm can cause a wide range of symptoms depending on where in the body it has occurred. This may include stroke-like symptoms:
- Fever
- Neck stiffness
- Confusion
- Aphasia, or difficulty speaking
- Numbness or weakness within certain areas, often on one side of the body
- Vision disruptions
- Difficulty walking
- Dizziness, loss of balance or coordination
- Severe headache
Cardiac vasospasms can mimic heart attack symptoms, including:
- Sharp or severe chest pain or pressure
Vasospasms affecting other areas of the body can result in:
- Sharp burning or stinging pain
- Fingers or toes turning purple or blue
How is vasospasm treated?
Vasospasm can be challenging to resolve, and so prevention is key. Ensuring patients are adequately hydrated and the use of nimodipine, a neuroprotective medication, can help reduce the likelihood of occurrence.
- Non-invasive neurologic monitoring via transcranial doppler (TCD) helps identify the condition’s early physiological signs by measuring the velocity of blood flow from the cerebral vessels most likely to be impacted.
- Increases in blood flow velocity indicate the onset of vasospasm, which triggers early interventions that can make all the difference for recovery. When identified too late, vasospasm can result in irreversible damage with long-lasting health impacts or death.
When vasospasm has developed, the focus becomes ensuring the brain is not deprived of oxygen. The medical team will artificially elevate blood pressure to facilitate blood flow, and administer additional neuroprotective medications, including mannitol and hypertonic saline. In many cases, endovascular procedures are recommended, including mechanical balloon angioplasty and intra-arterial medications to dilate blood vessels.