What People with Parkinson’s Disease Should Know about COVID-19
Internationally, April is the month we raise Parkinson’s disease (PD) awareness, but this year we cannot do that without acknowledgement of COVID and the impact it is having on the world.
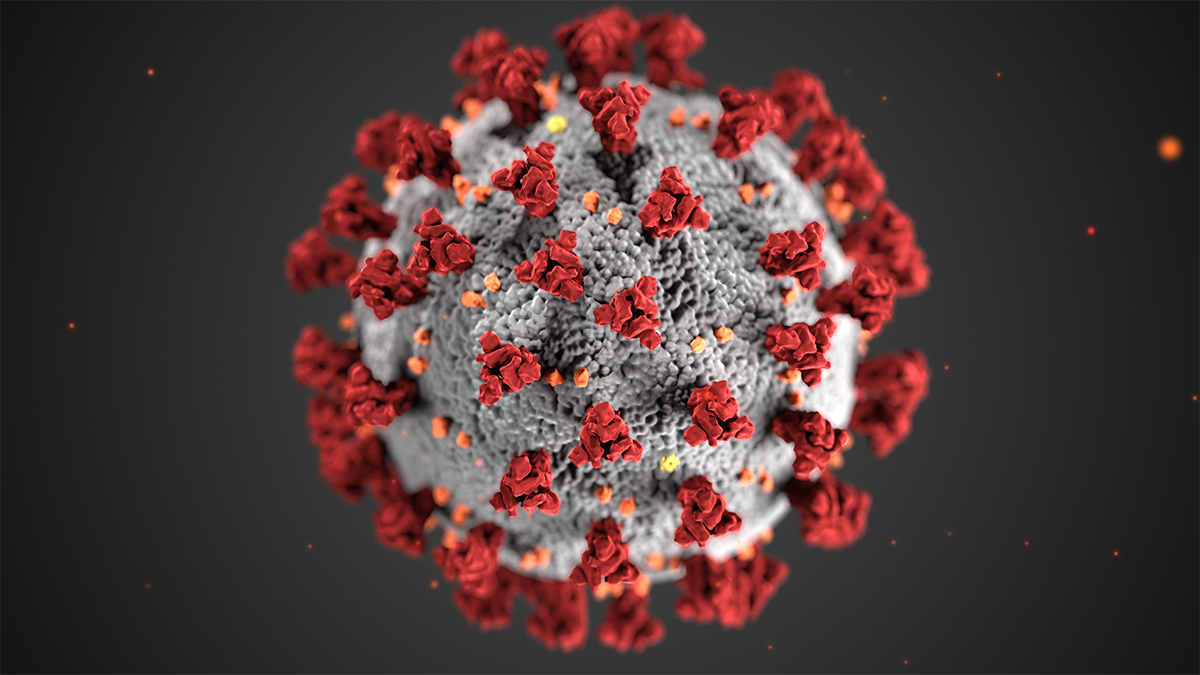
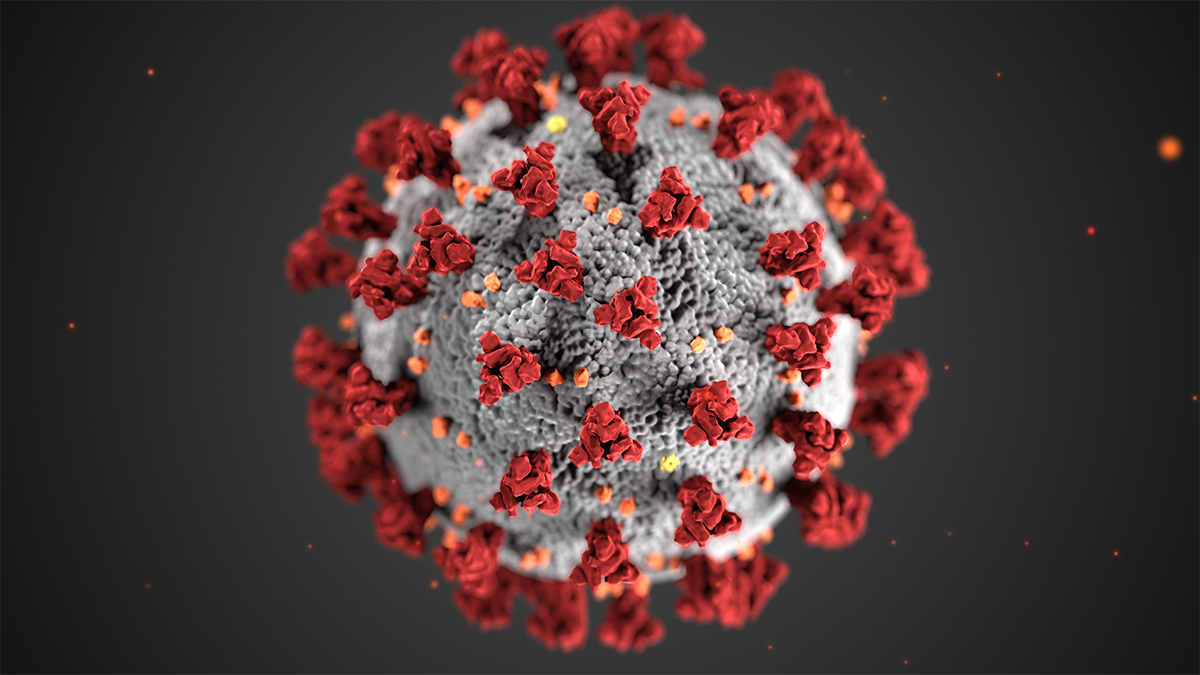
As of April 20th, at least 753,317 people in the U.S. have tested positive for COVID-19 and New Jersey has the second largest number of cases in the country. By way of background, coronaviruses have been around for a long time, and we know them intimately because they are a family of viruses that cause everything from SARS and MERS to the common cold. But COVID-19 is a particular strain of coronavirus that is a novel, or new, type of virus that humans currently have no immunity against. The reason it has been more dangerous, and more successful in spreading, is because it binds more tightly to certain receptors in the body, making it highly infectious. And studies are showing that for every one patient that may be symptomatic, there be up to eight asymptomatic carriers, making this silent enemy extraordinarily disruptive.
While you may have heard that individuals with a history of cardiac or lung disease are at greater risk for complications from COVID-19, it is important to recognize that Parkinson’s patients are also considered a high-risk group.
When coronavirus enters the lungs, it causes significant inflammation and buildup of fluid, making it difficult to breathe. Because all muscle movements slow down in people with Parkinson’s disease, the effects of COVID-19 compound the physical constraints a PD patient already has, making it more challenging to expand the lungs, take a deep breath and get enough oxygen. In addition, people with advanced Parkinson’s have difficulty swallowing and a poor gag reflex. That can increase the risk of aspiration pneumonia (a lung infection that occurs when you accidentally inhale food or liquid into your lungs). If you contract COVID-19 on top of having aspiration pneumonia, your already weakened lungs become even more compromised.
So, this raises the next question: what can you do to minimize your risk of exposure to COVID-19?
The first steps you should take to lower your risk of contracting COVID-19 are the same ones that people who do not have Parkinson’s disease are advised to take:
In addition to these steps, you should make sure you’ve gotten your pneumonia and flu vaccines and have a three-month supply of your medications on hand. To avoid the risk of exposure at the pharmacy, check to see if your insurance plan offers a mail order pharmacy option or if your local pharmacy delivers. If you have any non-urgent physician’s visits scheduled, ask to have a virtual visit via phone or video chat instead.
It’s also critical to stay physically active and keep your muscles moving, even when you’re isolating at home. Take a walk outdoors during an off-peak time of day. Gyms and rehab centers may be closed, but there are great videos on many websites that support the Parkinson’s community from yoga and cycling to LSVT exercises that you can do at home.