What is degenerative disc disease?
Degenerative disc disease is a condition marked by the wearing down of your spinal discs. Spinal discs are fluid-filled cushions between your vertebrae, which are the small bones that make up your spine. As cushions, these spinal discs do exactly what you would expect—they act as shock absorbers for the vertebrae and increase the flexibility of the spine.
With degenerative disc disease, these discs shrink and lose height due to dehydration. In their degenerated state, they may begin pressing on nerves or cause the vertebrae on either side to start rubbing together. As a result, some of the common conditions associated with degenerative disc disease are back pain, adult scoliosis, herniated discs, spinal stenosis, and spondylolisthesis.
What causes degenerative disc disease?
Degenerative disc disease is a common condition most closely linked with aging. In fact, about 30% of people show some signs of degeneration by age 35, increasing to 90% at age 60. The disease is specifically for people who not only have degeneration, but also experience the associated pain and other symptoms caused by the compromised discs.
Some of the factors that increase the likelihood of degenerative disc disease are: obesity, biological sex (women are more likely than men), smoking, ongoing and intense physical labor, poor posture, and acute injuries. Because degenerative disc disease is linked to the natural aging process as well as some specific factors that you can control, it’s often the case that there are multiple underlying causes.
What are the symptoms of degenerative disc disease?
Degenerative disc disease is closely associated with neck and back pain. Some of the specific symptoms, including the location of the pain, will likely depend on the part of the spine that is being affected. The condition may also cause weakness or numbness in your arms and legs if teh disc is herniated and causing pressure on the spinal cord or spinal nerves..
Some people find that the pain starts and stops, with some of the intervals lasting as long as weeks or months. It’s also likely that certain positions and postures will cause more or less pain: Bending, twisting, lifting, and sitting are common activities that exacerbate degenerative disc disease discomfort.
How is degenerative disc disease diagnosed?
Diagnosis usually begins with a conversation with your doctor about pain symptoms. They will likely ask about the location of the pain, any recent incidents or activities that instigated or exacerbate it, and whether there are any other symptoms (like numbness) in conjunction with the pain.
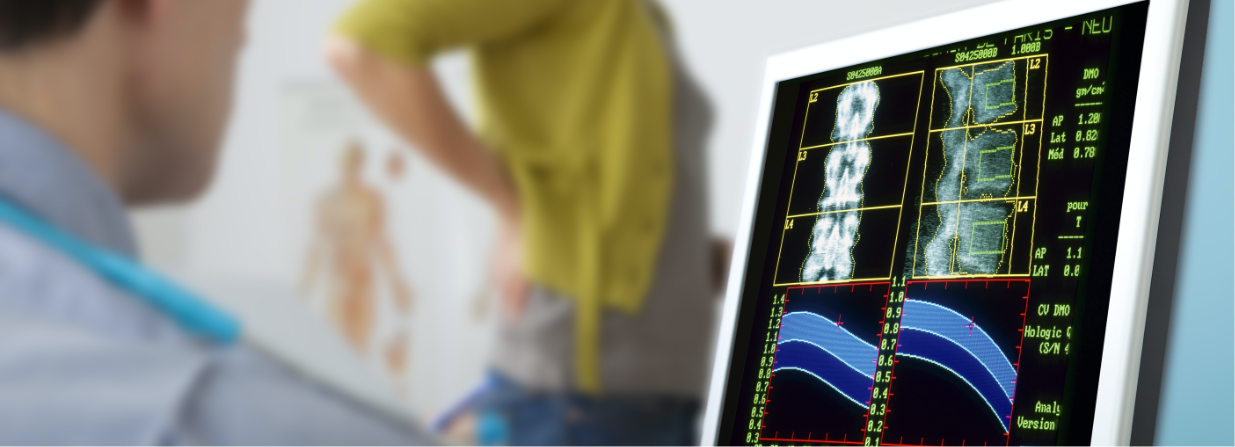
Then, your doctor may decide that imaging tests are a good next step to pinpoint the cause. An MRI scan can provide a detailed look at your discs, including whether they are pressing on any nerves or crowding the spinal canal. A CT scan is also a good option if you have metallic implants that prevent you from getting an MRI. A CT scan will show your doctor a detailed look at your spine’s structural integrity, as will an X-ray.
How is degenerative disc disease treated?
Working with a comprehensive spine center like ours can be a one-stop option for both diagnosis and a variety of treatment options, especially since treatment can vary so much for degenerative disc disease. Lifestyle changes, medication, physical therapy, and surgery may all be on the table, depending on the location and progression of the degeneration. While it is not possible to rehydrate the discs in your spine, you may be able to reduce the pain and relieve some of the pressure and other associated effects of the degeneration.
Weight loss, for instance, may lessen the pressure on your spine, and core strength can be a sizable factor in reducing back pain. Corset braces and cervical spine collars can also serve to lessen how much weight your spine has to bear in the places where your discs have shrunk.
Steroid medications and injections, as well as other oral pain management medications, may also be a good fit for periodic flare-ups.. Physical therapy is another good option, because specific stretches and exercises can build strength and relieve the pressure that causes pain.
When it comes to surgery, there are several procedures that your doctor may recommend. Spinal decompression surgery, spinal fusion surgery, and disc replacement surgery are options your doctor can talk through with you. Although surgery is often considered a last resort, the right procedure with an experienced surgeon can be safe, effective, and a means for improving quality of life.
Because degenerative disc disease is an umbrella term that often spans a range of more specific conditions, it’s important to understand all of the factors affecting your spine. The right diagnosis, followed by detailed conversations with your doctor, can set you on a path to pain relief.