There are more than 100 types of headaches. How do you know when your headache requires medical attention?
Headaches are one of the most common health complaints. And while many can be caused by stress, a cold, or the weather, a few types of headaches need medical attention as they can be symptoms of a more serious or life-threatening medical condition.
As a neurosurgeon, I treat brain aneurysms, strokes, and arteriovenous malformations (AVMs), all of which may involve head pain in some fashion. I am often asked, “How do I know if my headache is serious?” Here are some clues.
Headaches are a pain in the neck
Headache pain can have multiple causes. Tension headaches occur when the muscles of the scalp tighten up and compress the nerves of the skin, which often is felt as a sharp headache.
Other headaches may be due to irritation of the meninges, or the outer covering of the brain.
Migraine headaches are associated with blood vessel constriction over the brain surface, often with a warning symptom such as wavy vision, occurring minutes beforehand. A specific incident, such as a head injury or recent stroke, also can cause lasting headaches.
Other common causes of headache include infections or illness, such as the flu, cold, or sinus infection, as well as stress, dehydration, alcohol, allergies, strong odors, and some foods.
People are most familiar with tension and migraine headaches. Tension headaches are typically caused by stress. They cause moderate pain that is either sharp and focal or is spread equally around the head like a headband.
Migraines can be quite painful, even debilitating, and usually occur in a specific area of the head, such as behind the eyes or on just one side of the head. They are often accompanied by nausea or light sensitivity. When a migraine strikes, it can feel like something is severely wrong.
Sometimes, people with migraines fear they are suffering from a brain aneurysm, which is a bulge in the lining of a weak blood vessel that could burst and lead to fatal bleeding in the brain. The overwhelming majority of people with headaches do not have a serious underlying condition. Most of the time, it’s just a headache.
What’s the difference between a migraine headache and an aneurysm?
An aneurysm is a condition, whereas a headache is really the symptom of a condition. A brain aneurysm is a bubble, sac, or outpouching on the sidewall of a blood vessel. Brain aneurysms usually take years to develop and can slowly grow over time. A brain aneurysm usually causes no symptoms if it is small and has not ruptured or bled.
In some cases, symptoms of an aneurysm could include headaches, pain above or behind the eyes, facial numbness, blurry or double vision, or weakness. These symptoms are more common in people with migraines, as migraines are a much more common condition. We believe that approximately three percent of people have a brain aneurysm. The vast majority of these people will never experience a problem from the aneurysm, but a small number of people will. There are approximately 30,000 people who suffer a ruptured brain aneurysm per year in the U.S.
Usually, a brain aneurysm has no symptoms at all until it ruptures. When that happens, you’ll know it because, as some patients say, it comes out of nowhere (like a thunderclap) and feels like the worst headache you’ve ever had, by far. Migraines, on the other hand, tend to come on more gradually, usually over minutes to hours, with precursor symptoms, such as fatigue, nausea, or seeing visual auras. Tension headaches will also develop more gradually, over minutes or hours.
Knowing the difference between these conditions may offer some assurance of how urgently you need to take action.
Brain Aneurysm
An aneurysm starts off as a bulge in a weakened section in the wall of an arterial blood vessel. It often occurs in the brain but also can occur anywhere in the body. As blood flow puts pressure on this weak section of the blood vessel wall, the bulge grows out slowly, like a balloon, over time. Sometimes the aneurysm can suddenly burst, causing extreme headache, nausea, vomiting and life-threatening bleeding.
- Causes: Hardening of the arteries, certain genetic disorders, high blood pressure, or smoking.
- Symptoms: If not ruptured, there are usually no symptoms, or they are very mild, such as dull headache or blurry vision. If the aneurysm ruptures, severe pain occurs immediately, bringing on a sudden agonizing headache and often vomiting. A person with a ruptured brain aneurysm can suddenly lose consciousness and collapse. This is a true medical emergency.
- Risks: Stroke or massive internal bleeding, both of which can be fatal or debilitating if not treated immediately.
- Prevention tips: Manage high blood pressure well; exercise; get regular health exams; stop smoking. If you have a family history of a brain aneurysm, you should be screened with an MRI or CT periodically.
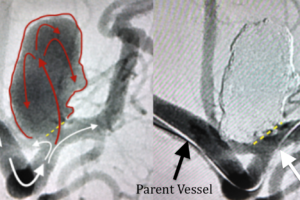
- Treatment: If you experience a sudden, severe, thunderclap headache, paralysis of one side of your face or body, or slurred speech, it’s imperative you call 911 or go immediately to an emergency room. The two most common treatment options for a ruptured aneurysm performed by a trained neurovascular surgeon are: 1) surgical clipping, in which the neck of the aneurysm is closed off with a small metal clip; and 2) endovascular coiling, which uses small catheters inserted through the leg and threaded into the aneurysm to place metallic coils and seal off blood flow to the aneurysm.
Unruptured aneurysm
It’s estimated that one in 30 people in the United States live with an unruptured brain aneurysm. Most of these people live normal lives, often not knowing they have one.
I need to emphasize that most patients with an unruptured brain aneurysm will never experience a problem from the aneurysm or even a headache from the aneurysm, but they do need to be fully evaluated by an expert. Typically, unruptured aneurysms are discovered incidentally during imaging or scans, such as an MRI or CT, for other medical conditions or neurological issues.
- Causes: Family history of brain aneurysms, age, gender (females are more prone), race, smoking, hypertension or some rare genetic disorders such as Marfan syndrome, Ehler-Danlos syndrome, sickle cell anemia, and adult polycystic kidney disease.
- Symptoms: Usually none, but can include headaches, dizziness, eye pain, vision problems, or seizures if the size of the aneurysm is large enough to cause brain or nerve compression.
- Risks: Rupture, which can cause a stroke or massive bleeding in the brain.
- Prevention tips: Control high blood pressure; stop smoking; eat a plant-based diet with whole grains; refrain from recreational drugs. If you have a family history of brain aneurysms, you may benefit from screening using an MRI or CT scan.
- Treatment: Observation, surgical clipping, endovascular coiling, flow diversion, or in rare cases, arterial bypass.
Migraine headache
The words “headache” and “migraine” seem to be used interchangeably a lot, but they are not the same thing. Migraines are a manifestation of a brain disease that requires a clinical diagnosis. They can occur episodically or chronically, are often disabling, and encompass accessory symptoms in addition to head pain.
- Causes: Exact causes of migraines have yet to be pinpointed, though genetics and environment may play a role. Family history, age, gender (females are three times more likely to suffer migraines), and hormones are factors.
- Symptoms: Pulsing or throbbing pain that occurs in one area of the head (such as just one side, front or back, around the eyes, or behind the cheeks); accompanying symptoms often include nausea or sensitivity to light, smell, or sound.
- Risks: Some correlations have been demonstrated between migraines and high blood pressure, heart disease, seizures, hearing loss fibromyalgia, and anxiety. In young women, migraines can increase the risks of certain types of strokes.
- Prevention tips: Be aware of environmental factors that can trigger migraines, such as bright or flashing lights, sun glare, and loud noises. Also pay attention to stress levels, weather, food choices (such as chocolate, red wine, processed meats), and changes in hormones.
- Treatment: Pain-relieving and preventive medications, Botox injections, antidepressants, anti-seizure medications. In some cases, you may benefit from seeing a headache neurologist for more advanced diagnosis and treatment of a migraine.
“…the vast majority of patients with a brain aneurysm will never experience a problem from the aneurysm or even a headache from the aneurysm, but they do need to be fully evaluated by an expert.”
– Reza J. Karimi, MD
When should you seek medical help for a headache?
Seek immediate medical help if your headache is unusually severe or grows worse, follows a head injury, or is accompanied by vomiting, fever, confusion, decreased alertness, a stiff neck, visual impairment, slurred speech, numbness, weakness, or seizures.
Call your physician if you notice:
- A major change in the pattern of your headaches.
- An unusually severe headache.
- A severe sudden onset “worst headache of your life.”
- A painful red eye.
- Interruptions of daily activity due to headache.
- An abrupt headache, especially if it wakes you from sleep.
Learn more about New Jersey Brain and Spine’s renowned Neurovascular Center here.